A stitch in time saves nine, they say — and a blood thinner in time saves a trip to the emergency room for a heart attack, as Diagnostic Robotics hopes to show. The company’s machine learning-powered preventative care aims to predict and avoid dangerous (and costly) medical crises, saving everyone money and hopefully keeping them healthier in general — and it has raised $45 million to scale up.
It’s important to explain at the start that this particular combination of AI, insurance, hospital bills and “predictive medicine” isn’t some kind of technotopian nightmare. The whole company is based on the fact that it’s both better for you and cheaper if you, for example, improve your heart health rather than have a heart attack.
That’s why your doctors tell you to cut down on red meat and maybe even take a cholesterol-maintenance medication instead of saying “well, if you have a heart attack just go to the ER.” It’s just common sense, and it also saves patients, hospitals and insurance companies money. And don’t worry, this kind of prediction can’t be used to raise your premiums or deny care. They want you making monthly payments — they just don’t want to have to shell out for a $25,000 operation if they can help it.
The question is, what about less obvious conditions, or ones that patients haven’t had specific tests for? This is where machine learning models come in; they’re very good at teasing out a signal from a large amount of noise. And in this case the AI was trained on 65 million anonymized medical records.
“We see how people look before the problems — everything we do is preventative care,” said Kira Radinsky, CEO and co-founder of Diagnostic Robotics. “It’s all about offering the right intervention, at the right time, to the right patient.”
She noted that providers often focus on the most expensive patients in order to reduce costs — for example, someone with advanced heart disease. But while acute and maintenance care continues to be important for them, that money has already gone out the door. On the other hand, if you diagnose someone with early signs of congestive heart failure, you can stop it from advancing and save money and possibly even a life. And the technique applies beyond things that can be detected in labs.
“Say the challenge is to find patients suffering from depression or anxiety, but aren’t taking any medications,” Radinsky proposed. “How do you identify someone with depression or anxiety based on medical records? We identify the entropy of their visits — lots of providers, lots of complaints — that’s a strong signal. Then you do specific questions, a medical triage, and you get them connected to a psychologist or psychiatrist, and they’re no longer deteriorating.”
The company claims it can reduce ER visits by three quarters, which is important beyond the immediate benefits for a person and their provider; ERs and urgent cares are overwhelmed in the U.S., paradoxically due to the pervasive fear of incurring huge medical expenses.
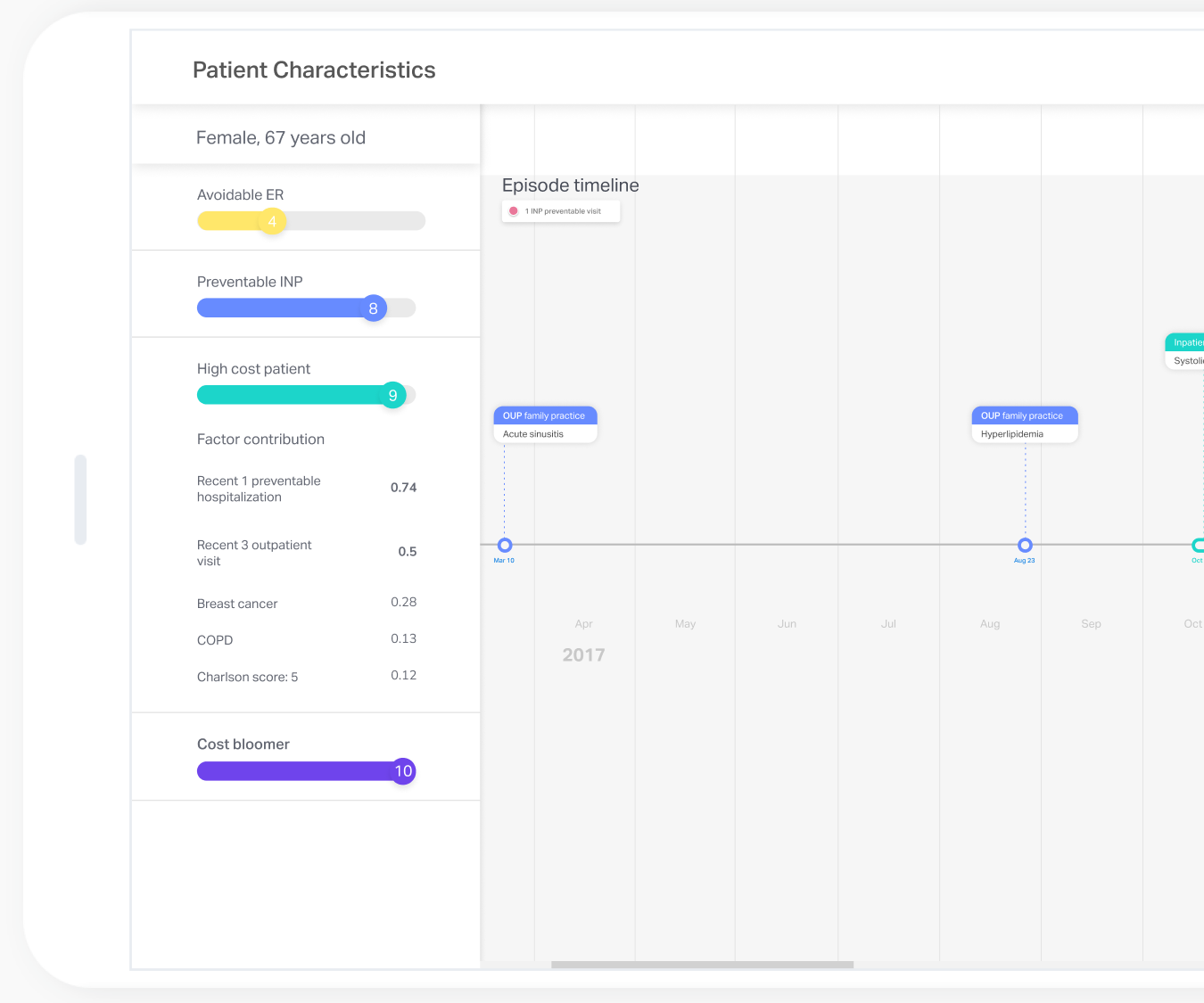
Example of a tablet interface showing a patient’s info as sorted by Diagnostic Robotics’ models. Image Credits: Diagnostic Robotics
Example of a tablet interface showing a patient’s info as sorted by Diagnostic Robotics’ models. Image Credits: Diagnostic Robotics
In many cases, she said, medical providers or insurers will offer medications or treatment for free or at nominal cost, because they know they’re saving themselves a bigger bill down the line. Sure, it’s all out of self-interest, but that means you can trust them.
The Tel Aviv-based Diagnostic Robotics just raised a $45 million B round, led by StageOne investors, with participation from Mayo Clinic, Technion (Israel Institute of Technology) and Bradley Bloom. Radinsky said this will help the company start working more directly with providers, taking on more holistic health goals in addition to specific high-risk conditions. (The company currently tracks around 20.)
A pilot test of this broader approach was recently validated in a study of a few hundred patients, in which the AI-prepared health plan was statistically indistinguishable from a clinician’s. The company is already serving millions of patients in some capacity, in Israel, South Africa and the U.S., with Blue Cross Rhode Island.
If they expand to your provider, don’t expect some kind of robotic examination, though the name obviously suggests this.
“You’ll get phone calls from care managers offering additional treatments, for free or almost for free,” Radinsky said. The AI will already have done its work, and maybe your test results and location suggest you’re at risk for something — and you’d do well to take these recommendations seriously. AI may have a lot of room to grow still but it’s good at sniffing out statistical correlations.
She was careful to add that they are also actively working on finding, defining and mitigating bias in the algorithms, whether it results from biased data or human error somewhere else along the lines. “What the algorithm is trying to do is see who will benefit the most,” Radinsky explained, but as with other forms of AI and machine learning, only careful monitoring will tell whether its idea of who benefits matches the real world.